Ventilators, virals, and vaccines
Disclaimer: This information is updated through June 1.
Ever since the COVID-19 began in China in December 2019, humanity has scrambled to find ways to treat the disease. When a novel disease emerges, treatment often comes in three steps: life support, anti-virals, and vaccines.
Mild cases
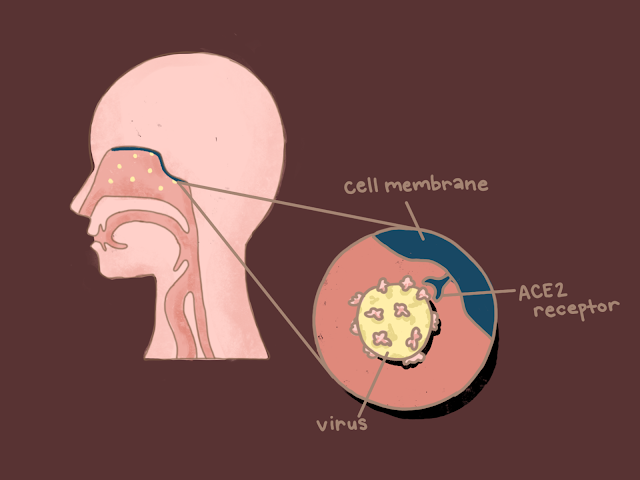
To understand how to treat a virus, it is important to understand its nature. As a virus, COVID-19’s sole objective is to reproduce and make copies of itself by infecting the human body, then transmit by bouncing from person to person.
During these first few hours of infection, the virus spreads from the air to the nose to the throat and the lungs. This is the disease’s incubation period, a time when the virus’s spread in the body is limited.
The onset of the disease is marked with mild symptoms similar to those of the common cold: fever, coughing, sore throats, etc. At this stage in the infection, common flu medicines like Tylenol can be used to treat the symptoms of the virus by suppressing the fever, clearing the throat, and making the sickness more bearable.
In fact, at this stage in the disease, fighting it off without any further treatment is plausible given how mild the symptoms are. Additionally, due to the state of healthcare facilities, with limited test kits and overburdened first responders, self-care at this stage is the medically recommended method to prevent further transmission.
Symptom progression
One of the mysteries of COVID-19 is its variability in impact. Some patients' symptoms are mild and dissipate with self-care. In other cases, however, symptoms worsen, often to the point of severe shortness of breath. The body then begins to work tirelessly to stop the advance of the virus. Symptoms of pneumonia begin appearing as the immune system tries to contain the virus. The infected lung cells become inflamed, secreting fluid to hinder the virus from spreading.
This viscous fluid coating lowers the amount of oxygen patients take in. Patients find it difficult to breathe and must gasp for breath. Those who test positive often get admitted to hospitals at this point, and their symptoms and a variety of conditions, such as blood oxygen levels, are monitored.
Internal levels of oxygen in the blood allow medical professionals to track how efficiently a patient is breathing. If the oxygen levels drop below 93 percent (only 93 percent of blood cells are saturated with oxygen), suffocation is imminent and patients are put on ventilators as life-support.
Lack of life-support
Due to their massive demand and medical necessity in saving advanced cases, ventilators have become increasingly hard to come by for those on the verge of suffocation. Medical manufacturing companies are working overtime to meet the ever-growing demand for ventilators. But they aren’t the ones producing these lifesaving machines.
President Trump has invoked the Defense Protection Act to increase the production of critical supplies. These quarantine laws are fairly new to all. “This is the first time in 50 years that quarantine laws have been used,” Scott Becker, CEO of the Association of Public Health Laboratories, tells Ishaan Shrestha from Silver Chips. “Generations of public health officials had never used this.”
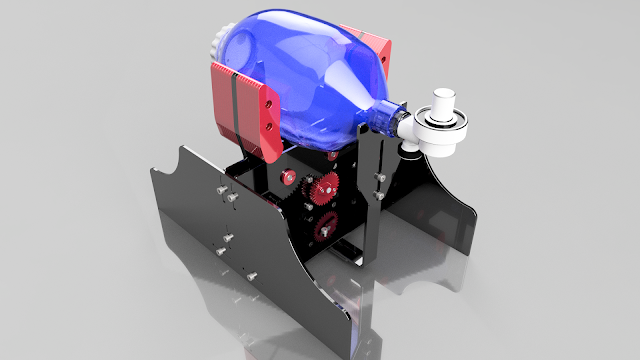
Although these quarantine laws are new for everyone, all walks of society are doing their best to help out. Car companies with large factories, mass production experience, and connections to the supply chains necessary for the hundreds of parts that go into a ventilator have done their best to adapt to the situation. General Motors received almost $500 million in government contracts to produce 30,000 ventilators by August. Similarly, Ford teamed up with GE Healthcare to produce 50,000 ventilators by July, and Tesla is repurposing its car parts to create its own model of a ventilator.
Since the FDA has loosened its regulations on ventilators, new models have been appearing all over the country. Universities like MIT and Vanderbilt are open-sourcing their designs, for instance, so that manufacturers around the world can use them.
Others aim to modify existing ventilators to be more efficient. Engineers from the University of South Carolina and medical engineering company
Prisma Health’s VESper ventilator project are sharing plans for a 3D-printed device that can allow one ventilator to be used on two patients.
Massachusetts General Hospital anesthesia residents are hosting the CoVent-19 Challenge, a contest for “rapidly deployable ventilator” designs to incentivize hobbyists and locals to join in the fight against the pandemic.
Even in high schools, students are searching for solutions to address the shortage. Some members of Blair’s robotics team have worked ventilator designs using computer-aided design (CAD) software.
Accessing anti-virals
Ventilators by themselves aren’t a cure to the disease. If symptoms worsen and no biological treatment is administered, intubation (invasive ventilators) may become necessary to ensure the proper flow of oxygen into the patient's bloodstream. However, the mortality rate at this point in the disease’s progression becomes very high as the immune system begins to lose control of itself.
The T and B white blood cells, the “commanders” of the immune system, control specialized Interleukin-6 (IL-6) white blood cells by marking which cells are healthy and which are viral. When the immune system begins to get overwhelmed with millions of viruses, the production of IL-6 spirals out of control, creating a “cytokine storm.
Overwhelmed with so many viruses, the cytokines (key proteins released by the immune system) lose the ability to properly recognize which cells are viral and the immune system begins attacking the body’s own organs. The immune system turns on itself, soon leading to organ failure.
In order to avoid this, hospitals have begun to administer different sets of treatments to patients before reaching this stage. The FDA has not approved any universal treatment, but dozens of experimental drugs are in the clinical trial stage of production.
Drugs deemed safe for clinical trials by the medical national Institutional Review Board––those not yet deemed safe for use by the general public––are tested on infected patients to ensure their effectiveness and monitor side effects. Each drug attacks a different part of the virus' reproduction process.
Hydroxychloroquine, the drug President Donald Trump has controversially endorsed due to the adverse effects noted by some studies, is one of many experimental drugs targeted at blocking the interaction between the virus and healthy cells. These types of drugs would ideally trigger a slowdown in the cell’s response to antigens, reducing the reproductive ability of the virus.
Remdesivir, another drug taking the media by storm due to its touted effectiveness, imitates the viral genetic material and sabotages the viral reproduction process, stopping the virus from spreading within the body. Existing drugs like Talampicillin and Lurasidone are being repurposed to prevent the virus from injecting its genetic material into the healthy cells in the first place.
Despite how well these solutions sound in theory, results from clinical trials are yet to be published, and safe, widespread commercial usage is still a ways off.
Looking at the long-term
For long term prevention, vaccines are needed to prevent another outbreak. Along with the clinical trials for drugs, clinical trials for vaccines have begun as well, with several labs across the globe gaining notable steps in the right direction.
Despite working toward similar goals, not all of these labs are taking the same paths, as dozens of vaccines are being produced through different methods: harvesting “elite” patients’ antibodies (injecting the antibodies from a patient who successfully fought off COVID-19 into another patient as medicine) or traditional dead viral presentation (injecting dead COVID-19 viruses into our immune system, like how the flu vaccine is delivered).
But since determining the effectiveness of a vaccine requires a very large sample size and long time frame, experts estimate that the earliest vaccines could be released to the general public within a year.
In the meantime…
As the disease continues to progress, we can stay informed by following the constant updates in the news.
“It's smart [that the] Maryland Department of Health and Mental Hygiene work very closely with local health departments like the Montgomery County Health Department to push out information in quarantine,” Becker from the Association of Public Health Laboratories says. “We can keep the mountain of American people informed through journalists.”
Everyone can do their part by staying informed, self-isolating, quarantining, washing hands, and maybe even participating in a ventilator contest.
Show comments
Comments
No comments.
Please ensure that all comments are mature and responsible; they will go through moderation.